Original article
Pattern of prescribing psychotropics in the outpatient department
of a tertiary psychiatric hospital
Mohammad Tariqul Alam,1 Mohammad Muntasir Maruf,2 Mekhala Sarkar,3 Helal Uddin Ahmed,4 Mahfuza Akhter5
1Assistant Professor, Department of Geriatric and Organic Psychiatry, National Institute of Mental Health (NIMH), Sher-E-Bangla
Nagar, Dhaka, Bangladesh; 2Assistant Professor, Department of Psychiatry, Shaheed M Monsur Ali Medical College, Sirajganj,
Bangladesh; 3Assistant Professor, Department of Forensic Psychiatry, NIMH, Dhaka, Bangladesh; 4Assistant Professor, Department
of Child, Adolescent and Family Psychiatry, NIMH, Dhaka, Bangladesh; 5 Senior Consultant (Skin &Vd) Shaheed Suhrawardy
Medical College Hospital, Sher-E-Bangla Nagar, Dhaka, Bangladesh.
Article info
Summary
Received
: 06 Oct. 2016
Pattern of prescriptions for psychiatric patients varies which is influenced by patient variation,
Accepted
: 01 Dec. 2016
types of disorders, cultural and environmental influences, socioeconomic status, availability of
Number of tables
: 04
drugs and psychiatrists own preference. The aim of this study was to determine the patterns of
Number of figures
: 02
prescribing psychotropic drugs in psychiatry Outpatient Department (OPD) in a tertiary care
Number of refs
: 17
hospital. The cross-sectional study was conducted in the OPD of National Institute of Mental
Health (NIMH), Dhaka from January to June, 2016. In the study, the prescriptions prescribed by
psychiatrists were considered as study population. Using convenient sampling method, data
were collected by observation using checklist from selected 604 latest prescriptions prescribed
by psychiatrists in OPD of NIMH for the patients coming there for treatment. The data on the
psychotropic drugs collected for the study were antipsychotics, antidepressants, mood stabilizers
and sedative-hypnotics. Results showed that a total of 1802 psychotropic drugs were prescribed
with an average of 2.98 psychotropics per prescription. The most common drug group prescribed
was antipsychotics (44.8%). Majority (49.7%) of the prescriptions contained 3 psychotropics
simultaneously. Most common (27.8%) combination was that of antipsychotics and sedative-
hypnotics. Dosage regimen was twice/day for the majority (55.6%). There was a combination of
oral and parenteral drugs in 48.3% of prescriptions. All the drugs were prescribed by brand
Correspondence
names. There was no diagnosis written in 60.9% of the prescriptions. The prescription pattern
Mohammad Tariqul Alam,
was not rational and this should be intervened by educating prescribers about rational prescribing
E- mail: sum.tariq@gmail.com
in psychiatry.
Bang J Psychiatry 2015;29(1):10-13
Introduction
It is important to realize that inappropriate use of drugs represent
Psychiatric disorders form an important public health priority. Of
a potential hazard to patients and an unnecessary expense.
the top ten health conditions contributing to the Disability Adjusted
This necessitates a periodic review of pattern of drug prescription
Life Years (DALYs), four are psychiatric disorders.1 Mental
to ensure safe and effective treatment.3 The rational use of
illness is associated with high level of health service utilization
drugs requires that “patients receive medications appropriate to
and associated costs, and in the developing countries, these
their clinical needs, in doses that meet their own individual
costs are mostly paid by the patient. Since 1950s, psychotropic
requirements for an adequate period of time, at the lowest cost
drugs have proliferated, and diagnosed cases have also
to them and their community”.4 The irrational use of drugs is a
increased. The expanding and challenging field of
problem, and to improve the overall drug use, especially in
psychopharmacology is constantly seeking new and improved
developing countries, international agencies like World Health
drugs to treat psychiatric disorders. In this way, psychiatrists
Organization (WHO) and International Network for Rational Use
are continuously exposed to newly introduced drugs that are
of Drugs (INRUD) have recommended standard drug use
claimed to be safe and more efficacious. Although psychotropic
indicators which help us to know the shortcomings in our
drugs have had a remarkable impact on psychiatry, their utilization
prescription writing.5,6 Drug prescribing pattern varies among
in actual clinical practice, effectiveness and safety in the real-
different geographical areas and is influenced by patient
life situation needs continuous study, and is thus a topic of
characteristics, type of disease prevalence, cultural and
increasing interest in recent times.2
Pattern of prescribing psychotropics in the outpatient department
Alam MT et al.
environmental influences, socioeconomic status, availability of
Results
newer drugs and prescribing habit of physicians. Describing
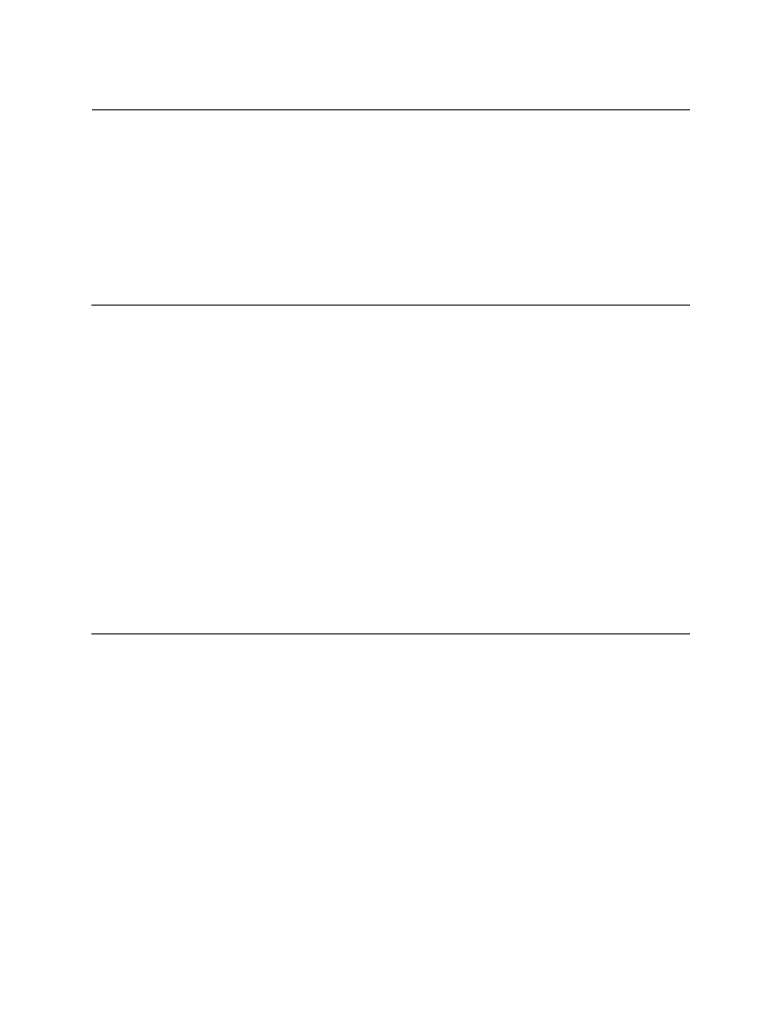
In majority (60.9%) of the prescriptions observed for the study,
drug use pattern and prescribing behavior, measurement of
no diagnosis was mentioned (Figure 1). There were 1802
drug use in the health facilities helps in identifying the factors
psychotropic drugs in 604 prescriptions with an average of
responsible for the practice of polypharmacy and the problems
2.98 psychotropics per prescription. Antipsychotics (44.8%)
associated with it.7 The study of prescribing patterns seeks to
were the most commonly prescribed psychotropics (Table 1).
monitor therapeutic trends, evaluate and if necessary, suggest
Among the prescriptions, only 58 (9.6%) contained one
modifications in prescribing patterns so as to make medical care
psychotropic. The rest 546 (90.4%) contained combination of
rational and cost effective.
psychotropics. Most (49.7%) of the prescriptions contained 3
psychotropics (Table 2). Among the combinations, antipsychotics
Many studies from the western countries have reported the
with sedative-hypnotics were the most common (27.8%)
prescription patterns of various psychotropic medications, which
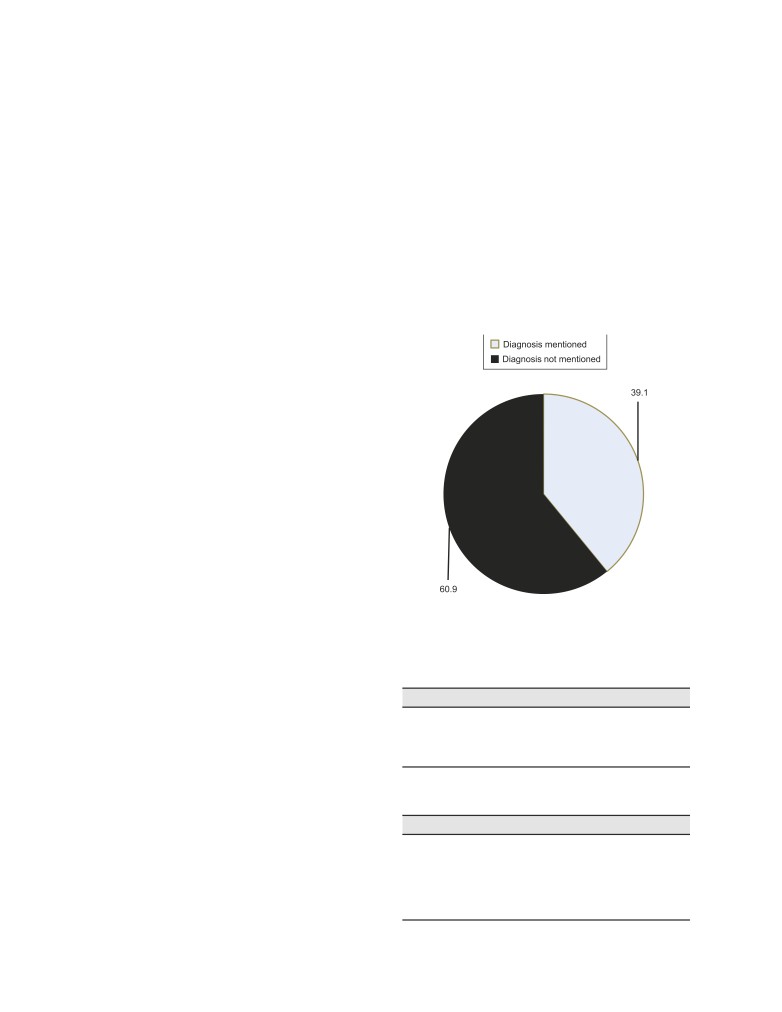
combination (Table 3). Most (83.8) of the psychotropics were
have looked into national prescription patterns, prescription
advised to take orally (Figure 2). Majority (55.6%) were advised
patterns in general practice, and specialist care, age, and gender
to take the psychotropics twice a day (Table 4).
differences in antipsychotic prescription, prescription patterns
of anti-depressants, mood stabilizers in bipolar disorder patients,
and rate of use of anti-cholinergic agents in psychiatric patients.
A few surveys of prescription patterns of various psychotropics
from Asian centers are available too.8-10
As there is no sufficient data available on their use in the
population of Bangladesh, the present study was carried out to
observe the patterns of prescribing psychotropic drugs in
psychiatry outpatient department.
Materials and methods
It was a hospital-based cross-sectional study. The study was
conducted over a period of six months from January to June
2016 at the outpatient department of National Institute of Mental
Health (NIMH), Dhaka, Bangladesh. The prescriptions prescribed
by psychiatrists were considered as study population. All
prescriptions having at least one psychotropic drug were
included. Prescriptions in which hand-writing could not be
Figure 1: Diagnosis mentioned in the prescription
understandable, or advised for admission, and referred to other
(n=604)
hospitals were excluded. Permission of the institutional ethics
committee was obtained for conducting the study. Informed
Table 1: Commonly prescribed group of psychotropics
consent was taken from all participants prior to their inclusion
(n=1802)
into the study. Using convenience sampling method, data were
Psychotropics
Frequency
Percentage
collected by observation using checklist from selected 604 latest
prescriptions prescribed by psychiatrists in OPD of NIMH for the
Antipsychotics
808
44.8
patients coming there for treatment. The sampling frame was
Antidepressants
246
13.7
Mood stabilizers
296
16.4
fixed as six prescriptions per day, five days a week, during the
Sedatives-hypnotics
452
25.1
sampling period. The six prescriptions were selected as follows:
On day 1, all six prescriptions were chosen from the first two
Table 2: Number of psychotropics per prescription
hours of the OPD, on day 2 six prescriptions were chosen from
(n=604)
the middle 2 hours and on day 3, six prescriptions were chosen
Number of psychotropics
Frequency
Percentage
from the last 2 hours of OPD and so on. In case of Out Patient
1
58
9.6
Department holidays, the prescriptions of that day were assigned
2
102
16.9
to the next working day. Data were analyzed using Statistical
3
300
49.7
Package for Social Sciences (SPSS) version 16. The
4
92
15.2
psychotropic drugs included for analysis were antipsychotics,
5
40
6.7
antidepressants, mood stabilizers and sedative-hypnotics.
6
12
1.9
11
Bang J Psychiatry
Vol. 29, No. 1, 2015
Table 3: Combination of psychotropics (n=546)
Combination
Frequency
Percentage
Antipsychotics+ Sedative-hypnotics
152
27.8
Antipsychotics+ Mood stabilizers
40
7.3
Antipsychotics+ Antidepressants
24
4.4
Antipsychotics+ Mood stabilizers+ Sedative-hypnotics
104
19.0
Antipsychotics+ Antidepressants+ Sedative-hypnotics
28
5.1
Antipsychotics+ Antidepressants+ Mood stabilizers
18
3.3
Antipsychotics+ Antidepressants+ Mood stabilizers+ Sedative-hypnotics
56
10.3
Antidepressants+ Mood stabilizers+ Sedative-hypnotics
24
4.4
Antidepressants+ Mood stabilizers+
14
2.6
Antidepressants+ Sedative-hypnotics
62
11.4
Mood stabilizers+ Sedative-hypnotics
24
4.4
males were represented with more psychiatric illness, compared
to females; this finding was contrary to the findings of Thakkar
KB et al. and Mant A et al.10,12
The age group of 26-35 years was found to be represented
with maximum psychiatric disorders. Here, we found that
antipsychotic drugs were the most commonly prescribed
categories of psychotropic medications followed by sedative
hypnotics, mood-stabilizers and anti-depressants in decreasing
order. The average number of psychotropic drugs per
prescription was 2.98, which was higher than that found in
similar studies, where it ranged from 1.79 to 2.5 drugs per
prescription.13,14 Average number of drugs per prescription
was an important index of prescription audit. It is preferable to
keep the mean number of drugs per prescription as low as
possible because multiple drugs lead to increased risk of drug
interaction. Out of the 604 prescriptions monitored in our study,
90.4% were prescribed more than one drug, 49.7% patients
were prescribed three drugs; we can say that polypharmacy
Figure 2: Route of administration of psychotropics
was not avoided. Polypharmacy can lead to poor compliance,
prescribed by psychiatristss (n=1802)
drug interaction, adverse drug reactions, under-use of effective
treatments, healthcare costs, and medication errors.15 In this
Table 4: Dosage regimen/day in prescription(n=604)
study, we found that the most common combination of drugs
Dosage
Frequency
Percentage
was of antipsychotics and sedative-hypnotics, followed by
antipsychotics, mood stabilizers and sedative-hypnotics.
Once
36
6.0
Twice
336
55.6
No drug was prescribed by generic names; contrary to the
Thrice
232
38.4
findings of the study done by Thakkar KB et al.10 There might be
no obligation of prescribing generic names among the medical
Discussion
practitioners at government tertiary care teaching hospital as
per local health administration order. It is against the WHO
A prescription may be taken as reflection of physician’s attitude
guidelines, where generic prescription is one of the indicators
to the disease and the role of drug in its treatment. It also provided
of rational prescribing. Generic drug prescribing also facilitates
an insight into the nature of the healthcare delivery system.11
cheaper treatment for the patient.
The present study aimed to analyze the current prescribing
pattern of psychotropic medications in the OPD of a tertiary care
The oral (83.8%) and parenteral (16.2%) preparations used in
psychiatric hospital. The demographic analysis suggested that
this study were comparable with those of Rode SB et al. and
12
Pattern of prescribing psychotropics in the outpatient department
Alam MT et al.
Dutta SB et al.16,17 The injection most frequently prescribed
5.
World Health Organization. How to Investigate drug use in
health facilities: selected drug use indicators. Geneva: World
was fluphenazine decanoate (25 mg) intramuscularly. Concerns
Health Organization; 1993.
about the adverse effects and cost-effectiveness of the
6.
World Health Organization. Drugs and therapeutics
parenteral route of drug administration are probably the reasons
committees - a practical guide. Geneva: World Health
for the low utilization of depot injection formulation in the
Organization; 2003.
psychiatry OPD.
7.
Gupta N, Sharma D, Garg SK, Bhargava VK. Auditing of
prescriptions to study utilization of antimicrobials in tertiary
No diagnosis was written in more than half (60.9%) of the
hospital. Indian J Pharmacol 1997;29(6):411-5.
prescriptions. The appropriateness of prescription of the
8.
Nakao M, Takeuchi T, Yano E. Prescription of
psychotropic drugs with regard to the diagnosis and co-
benzodiazepines and antidepressants to outpatients
morbidities was not evaluated in study. The factors such as
attending a Japanese university hospital. Int J Clin
cost, patient compliance, and adherence to treatment guidelines
Pharmacol Ther 2007;45(1):30-5.
while prescribing were not as well assessed. The study involved
9.
Piparva KG, Parmar DM, Singh AP, Gajera MV, Trivedi HR.
patients attending the OPD of a tertiary care psychiatric hospital
Drug utilization study of psychotropic drugs in outdoor
patients in a teaching hospital. Indian J Psychol Med
in the capital of Bangladesh; thus, the results cannot be a
2011;33(1):54-8.
representative of national data. The hospital resources (e.g.,
10.
Thakkar KB, Jain MM, Billa G, Joshi A, Khobragade AA. A
availability of free medicines from hospital) that might govern the
drug utilization study of psychotropic drugs prescribed in
issue of polypharmacy have not been considered in this
the psychiatry outpatient department of a tertiary care
research.
hospital. J Clin Dagn Res 2013;7(12):2759-64.
11.
Laporte JR. Towards a healthy use of pharmaceuticals. Dev
Conclusion
Dial 1985;2:48-55.
Though there are some limitations in the study, this can be
12.
Mant A, Lansbury G, Bridges-Webb C. Trends in psychotropic
concluded that the prescription patterns were not rational.
drug prescribing in Australia. Med J Aust 1987;146(4):
Diagnosis was not mentioned in most of the prescriptions and
208-10.
use of combination of drugs was remarkable. This issue should
13.
Lahon K, Shetty H, Paramel A, Sharma G. A retrospective
drug utilization study of antidepressants in the psychiatric
be intervened by educating prescribers about rational prescribing
unit of a tertiary care hospital. J Clin Diagn Res
in psychiatry.
2011;5(5):1069-75.
References
14.
Al Khaja KA, Al-Haddad MK, Sequeira RP, Al-Offi AR.
Antipsychotic and anticholinergic drug prescribing pattern
1.
Murthy RS. Mental health programme in the 11th five year
in psychiatry: extent of evidence-based practice in Bahrain.
plan. Ind J Med Res 2007;125(6):707-11.
Pharmacol Pharm 2012;3(4):409-16.
2.
Davidson JR, Feltner DE, Dugar A. Management of
15.
Bushardt RL, Massey EB, Simpson TW, Ariail JC, Simpson
generalized anxiety disorder in primary care: identifying
KN. Polypharmacy: misleading, but manageable. Clin Interv
the challenges and unmet needs. Prim Care Companion J
Aging 2008;3(2):383-9.
Clin Psychiatry 2010;12(2): PCC.09r00772.
16.
Rode SB, Ajagallay RK, Salankar HV, Sinha U. A study on
3.
World Health Organization [Online]. [cited 2003]; Available
drug prescribing pattern in psychiatry out-patient department
from a tertiary care teaching hospital. Int J Basic Clin
drug_utilization_research.pdf
Pharmacol 2014;3(3):517-22.
4.
De Vries TPGM, Henning RH, Hogerzeil HV, Fresle DA.
17.
Dutta SB, Dhasmana D, Bhardwaj R. Psychotropic drug
Guide to good prescribing: a practical manual. Geneva:
utilization pattern among patients with schizophrenia.
World Health Organization; 1994.
Indian J Psychiatry 2005;47(4):243-4.
13